Patient Experience
Eastern Health seeks to hear the voice of the patient, families and carers in a number of different ways. Patients, families or carers can:
- Speak with any staff member or the manager from the area where the experience occurred;
- Call, email or write to the Centre for Patient Experience;
- Use feedback forms in feedback brochures found in patient areas;
- Use the online feedback form on the Eastern Health website;
- Publish your experience without giving your name on the online public platform Care Opinion; and
- Complete the Eastern Health Patient Experience Survey available on discharge.
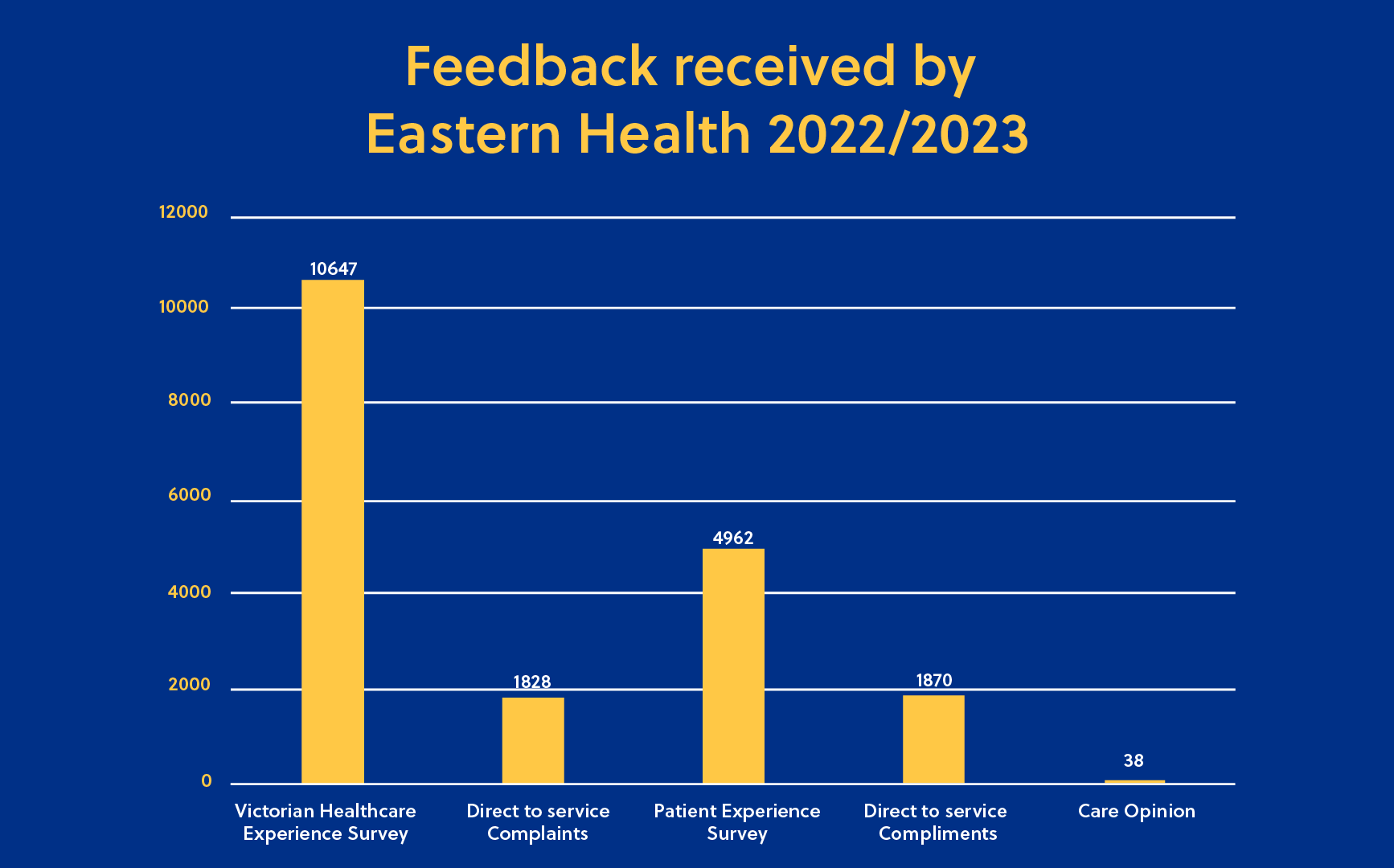
There were 19,345 items of feedback received by Eastern Health in 2022/2023. The mechanisms used for feedback in the past year are shown below.
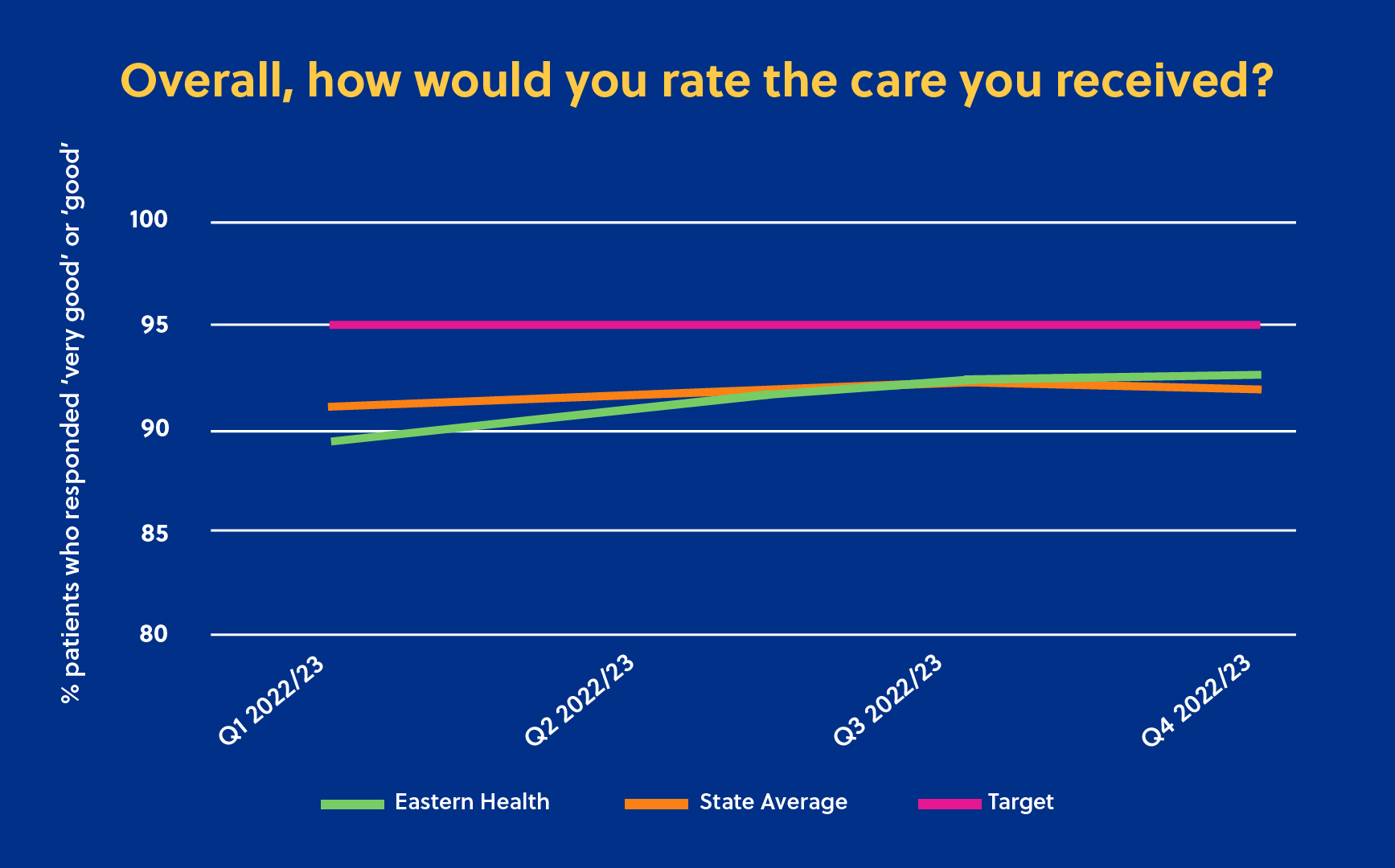
The Victorian Healthcare Experience Survey (VHES) is one of the ways patients can provide feedback about their experience with Eastern Health. The VHES collects information from a range of healthcare users of Victorian public health services. The survey is conducted by Ipsos (on behalf of the Department of Health & Human Services), and invites feedback from patients after discharge from the Health Service. The table below provides responses from Adult Inpatients at Eastern Health during 2022/23 to the question “Overall, how would you rate the care you received?”. Eastern Health’s performance improved steadily each quarter with performance equal to the state average for quarter 3 and above state average for quarter 4.
Eastern Health uses feedback from patients to identify opportunities to improve our services and the experience of patients, carers and families. Below are some examples of taking action based on feedback provided by consumers.
|
You said (the patient) |
We did (what actions we have taken from the feedback) |
| I’m not sure what queue I’m meant to line up in when I get to the Emergency Department. It seems disorganised and like there is no system | Box Hill Emergency Department commenced a ‘sift and sort’ model of care whereby a triage nurse streams patients arriving to the Emergency Department using a workstation on wheels. Patients are asked to briefly describe their reason for presenting and are then advised of where to wait for formal triage. |
| The seating in the waiting areas at Healesville Hospital is not supportive enough. |
New seating has been provided which provides more support. |
| It is not good enough that Auslan interpreters aren’t available to provide onsite interpreting. | We have moved to a new service provider for Auslan Interpreting who have a wider range of services and have been able to provide onsite interpreters. |
Partnering with Consumers
The “Preparing for Home Envelope” aims to ensure patients and their families and carers have been provided relevant information, equipment and support prior to discharge home. The envelope is designed for patients to complete in conjunction with their treating team and has spaces to fill in patient specific information. It also provides QR codes to key resources such as the Partners in Care Booklet, the Eastern Health Patient Experience Survey, and the feedback section of the Eastern Health website. In 2023, Eastern Health has been piloting the envelope across two inpatient wards at Box Hill Hospital. Feedback to date has been very positive from both patients and staff.
|
You said (the patient) |
We did (what actions we have taken from the feedback) |
| In the Eastern Health Patient Experience Survey 78% of patients responded “Yes-definitely” to the question “Did you feel that you were given all necessary information about how to manage your health and care at home?” | We are piloting a “Preparing for Home Envelope” which aims to ensure patients and their families and carers have been provided relevant information, equipment and support prior to discharge home. |
In early 2023, Eastern Health rolled out a communication campaign to promote the ‘Question Builder’ resource to consumers. Question Builder is a free online tool developed by the Australian Commission for Safety and Quality I Healthcare in partnership with Healthdirect Australia. It helps consumers think about the questions they might like to ask their health professional and to prepare for questions health professionals may ask them when they go to an appointment.
|
You said (the patient) |
We did (what actions we have taken from the feedback) |
| I leave my appointment and then remember all the questions I wanted to ask! | Eastern Health ran a campaign to promote the Question Builder resource – a free online tool to help you think about the questions you might like to ask your health professional, and to prepare for questions health professionals may ask you when you go to an appointment. |

Family members and carers are ideally placed to identify early, and often subtle, signs of clinical deterioration. This is due to:
- their familiarity with the patient, which helps them to see early changes in behaviour or other signs of illness
- the period of time families or carers usually spend with their loved one, enabling them to see signs of decline that the healthcare team might not see.
Eastern Health has a three-step escalation process that allows patients, families and carers to initiate an escalation of care for their loved one in hospital when they are not doing as well as expected or not improving, or there is concern that the patient’s condition is getting worse. Details of this process are available here
In 2023, ‘Parental escalation’ brochures were introduced. The brochures are given to all parents and carers of children presenting to triage at Eastern Health Emergency Departments and/or admitted to the Paediatric Ward at Box Hill Hospital. These brochures include visual prompts about detecting deterioration in children and outline how to escalate concerns.
Diversity
In early 2023, a new Diversity Equity and Inclusion Committee was formed to provide governance and leadership in ensuring Eastern Health is an inclusive and culturally safe service, responsive to Diversity, Equity and Inclusion for consumers, the community and staff.
Eastern Health is committed to ensuring a safe workplace and to being an inclusive provider of healthcare for all lesbian, gay, bisexual, trans and gender diverse, intersex, and queer and questioning (LGBTIQ+) people. The Rainbow eQuality Working Group working has supported a number of initiatives including:
- An Eastern Health contingent at the Pride March 2023
- Coordinating communication and acknowledgment of “Wear it Purple Day” and “IDAHOBIT Day” (International Day Against Homophobia, Biphobia, Intersexism and Transphobia);
- Ad hoc training and awareness sessions to address issues raised by patients and staff regarding the needs of LGBTIQ+ people.
|
You said (the patient) |
We did (what actions we have taken from the feedback) |
| Results in the Eastern Health Patient Experience Survey demonstrated that patients who identify as LGBTIQ did not feel as respected as patients who do not identify as LGBTIQ and did not feel individual needs were considered as much as patients who do not identify as LGBTIQ. | We have employed LGBTIQ+ Liaisons to work with patients, families, carers, and staff to drive systemic change to improve health access, outcomes and experiences for our LGBTIQ+ community. |

In 2023/23, the Eastern Health Disability Working Group has continued to undertake work to oversee and support the implementation of actions on the Disability Action Plan. Eastern Health’s Disability Liaison Officers have supported the Working Group with key achievements in 2022/23 including:
- An average of 40 referrals per month to support people with disability to access healthcare to improve experiences and outcomes.
- Disability Car Parking audits of all hospital sites completed.
- Development of a Disability iLearn HUB to support staff with resources and tools.
- In partnership with Expressions and Deaf Victoria, significant improvements have been made to support access for patients, families and carers who are deaf.
- Piloting a Disability Health Passport in collaboration with Peninsula Health and 5 other health networks.
- Development of a NDIS 14 step clinical pathway to provide a method to ensure consistency, transparency and identification of barriers in supporting inpatients who are NDIS participants to access supports to ensure a timely discharge.
- Consultation and education with staff across EH to support the needs of people with disability.
|
You said (the patient) |
We did (what actions we have taken from the feedback) |
| I find disability car parking too difficult to access. |
We undertook a disability car park audit at each of our sites. We have doubled the number of Designated Accessible Parking Bays in the Davey Drive Visitor Car Park at Maroondah Hospital. |
Eastern Health is committed to continually improve and support Cultural Safety in our care and ensure we have a welcoming and supportive environment for Aboriginal and Torres Strait Islander peoples in our region. Maintaining and building relationships is integral to this. In late 2022, Eastern Health established the Aboriginal Health Advisory Committee. This Committee meets quarterly and provides strategic advice to Eastern Health on new and existing initiatives. The Committee has representatives from the Wurundjeri, Consumer representatives and representatives of the Aboriginal Community Controlled Organisations and Aboriginal Community Controlled Health Services in our region.
Support for Aboriginal patients has grown at Eastern Health in 2023, with the expansion of the Aboriginal Hospital Liaison Officer Program. This program now has a Team Leader role and two additional AHLO positions so that cultural support is available across every Eastern Health site. An ongoing focus of the organisation has also been to enhance our Cultural Safety Training. In 2022, Eastern Health partnered with AJ Williams from Girraway Ganyi who has delivered several Cultural Insights workshops to staff in our Emergency Departments, Women and Children Program and staff in Quality Improvement and Clinical Governance. Eastern Health continues to celebrate and acknowledge significant days throughout the year, including National Close the Gap Day, Sorry Day, National Reconciliation Week, NAIDOC Week and National Aboriginal and Torres Strait Islander Children’s Day. Eastern Health was proud to launch its Aboriginal Cultural Safety Plan – Healthier Together Towards 2024, outlining a significant program of work to support closing the gap, and improving our partnership with the Aboriginal Community at Eastern Health.

Consumer, carer and community participation
Eastern Health values the role that consumer voice and lived experience plays in shaping decisions about healthcare at the level of the system, service and individual.
Consumer representatives come from all walks of life and by sharing their experiences, help to keep the needs of health service users at the front and centre.
Consumer representatives partner with Eastern Health by participating in a range of committees, working groups, consultations, research, improvement projects and staff training.
- Developing a training module to support undertaking Gender Impact Assessments
- Consultation on the design and development of the new EH website
- Working with different Eastern Health teams to support communications and awareness days including NAIDOC Week video and Trans and gender diverse awareness panel
- Reviewing patient education resources
- Membership on many new committees including the Digital Health Plan Steering Committee and the Eastern Health Emergency Services Improvement Steering Committee
- Involved in many new projects and working groups including Timely Emergency Care, Supportive care screening for oncology patients, and the Peripheral Intravenous Cannula Governance Group
Consumer representatives also partner on behalf of Eastern Health by attending and contributing at many external events run by Safer Care Victoria and other peak bodies and consumer organisations.
- Attending the Patient Associations Awards
- Presenting at the Partnering in Healthcare Outcome Summit
- Partnering with Healthcare Organisations project
- Victorian Health Consumers Community of Practice
- Co-authoring on posters and journal articles
Eastern Health’s Response to the Royal Commission into Victoria’s Mental Health System
Eastern Health’s Mental Health and Wellbeing Program is reforming services to ensure alignment with the recommendations from the Royal Commission into Victoria’s Mental Health System.
- The operationalisation of a new community clinical sites in Forest Hill and Ringwood
- Implementation of a significantly expanded junior allied health and nursing workforce model to support our long-term workforce growth requirements, and
- Recruitment to our inaugural Associate Program Director of Lived Experience facilitating improved consumer and family engagement in service design and delivery.
- increase services at times when they are needed
- have people who understand the consumer and family experience first-hand
- support daily health and wellbeing as well as mental health needs and improve care for people living with both mental health and substance use concerns.
Quality and Safety Outcomes
An incident is an event or circumstance which could have resulted, or did result, in unintended or unnecessary harm to a person receiving care.
Each incident is rated according to degree of harm and changes to the level of care and treatment required as a direct result of the incident. This severity rating informs follow up of both the individual incident and system issues identified. Each incident is assigned a rating between 1 and 4, 1 being the most serious outcome to 4 where no harm has occurred but was a near miss.
All reported incidents are initially reviewed by the manager of the location where the incident occurred. There is an immediate assessment of safety and care of those involved and any identified concerns are addressed. Information is gathered from staff, patients and visitors at the time of the event to get a thorough picture of what has occurred.
All incident reviews apply the following key principles:
- Determine the timeline of events leading up to an including the incident
- Identify if there are any issues/ variations from expected practice
- Identify what may have contributed to the issues.
- Consultation and communication with the patient/family to ensure a collaborative and informed process.
The most serious incidents are reviewed by a panel of clinicians, service providers and consumers.
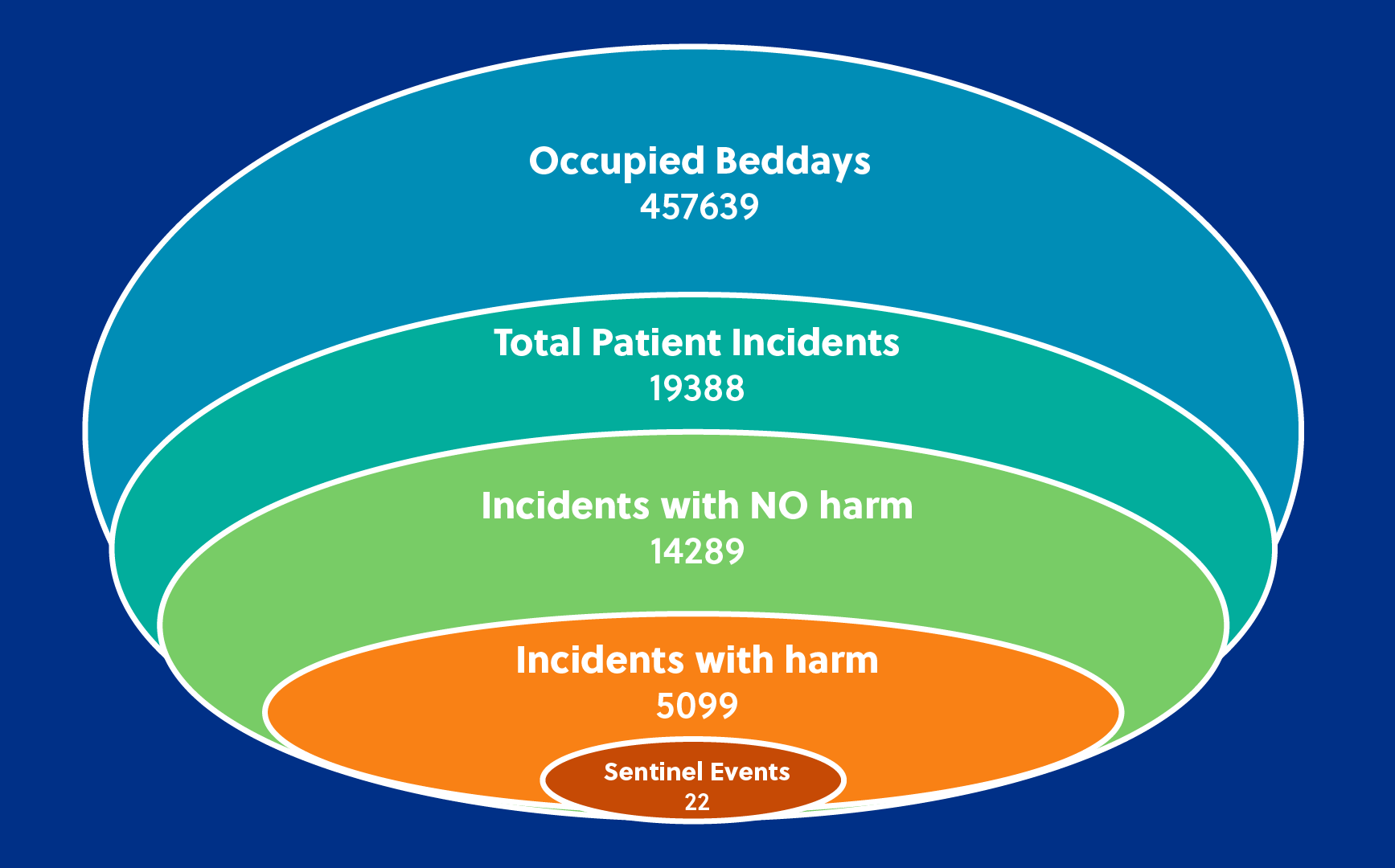
Sentinel events are unexpected events that result in death or serious harm to a patient while in the care of a health service. Eastern Health notified SCV of 22 sentinel events during 2022/23.
- Graphic demonstrating incidents numbers with and without harm
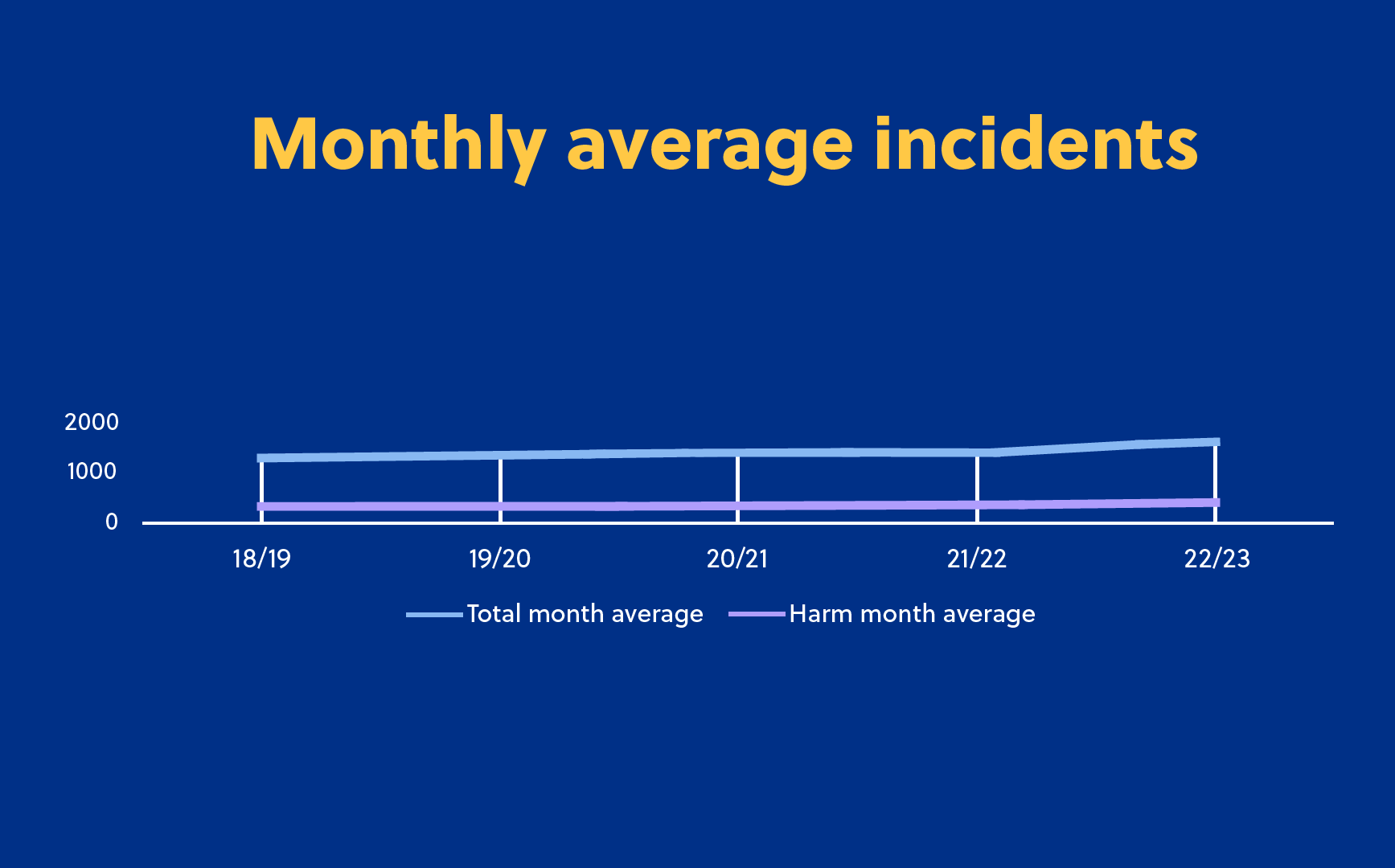
- Incident numbers by month
- Average of 1615 patient incidents are reported per month
- Average 424 patient incidents resulting in harm are reported per month
- The three main incident types where harm has been experienced by a patient are:
- Falls (3480 in 2022/2023);
- Behaviours of concern* (7595 in 2022/2023); and
*Behaviours of Concern are behaviours that people engage in which are unsafe and/or distressing to the person and/or others. This may include someone harming themselves, other people or things. These behaviours can be very stressful and upsetting. These behaviours can seriously hurt people.
- Skin integrity (for example, bed sores or skin breaks) (1377 in 2022/2023)
- Improvements
The primary purpose of incident review is to understand how and why the incident occurred and to identify ways of preventing recurrence. Here is an example.
Case 1
|
What happened? |
What did we do? |
|
A consumer experiencing a deterioration in mental state ingested two AAA batteries obtained from the in-patient ward’s television remote control. An abdominal x-ray confirmed location of batteries with a gastroscopy procedure undertaken to remove the batteries. |
In the short term, the television remote control was super glued shut and a number of universal remotes were purchased to ensure availability of remote when batteries lost charge. Following a review of available products suitable for this high risk environment, an iPad product has been selected for trialling. |
Incident numbers are increasing year on year. There are a number of variables that contribute to the rise including expansion of services and therefore increased numbers of consumer contacts. The percentage of these incidents that relate to harm however has remained stable over the 5 years illustrated.
Outcomes from other areas
On the 30 November 2022, the Statutory Duty of Candour came into effect following changes to the Health Legislation Amendment (Quality and Safety) Act 2022. Eastern Health has a legal and ethical responsibility to maintain open, honest and empathic communication with patients, families and carers – our consumers. This includes when an adverse event or unexpected outcome has occurred. In addition, if a patient experiences a serious adverse patient safety event (SAPSE) in the course of receiving services the Victorian Statutory duty of candour (SDC) applies. SDC is a legal obligation for Victorian Health service entities to ensure that patients/clients/residents and their families or carers are apologised to and communicated with openly and honestly when a SAPSE has occurred. It builds on the Australian Open Disclosure Framework currently utilised for all cases of adverse patient safety events including near misses. Communicating in this way helps patients, families and carers to understand the impact of adverse events and facilitates the building of a relationship of trust between them, their clinicians and the organisation.
When a patient has suffered a SAPSE, Eastern Health is legally required to provide the patient, and/or their next-of-kin (NOK)/carer, with:
- a written account of the facts regarding the SAPSE
- an apology for the harm suffered by the patient
- a description of the Eastern Health’s response to the event
- the steps that Eastern Health has taken to prevent re-occurrence of the event.
From 30 November 2022, when the legislation commenced, until 30 June 2023 Eastern Health reviewed 53 SAPSE and of these 35 consumers accepted the SDC process. Following completion of the SAPSE process, consumers are invited to complete an evaluation survey.
Eastern Health demonstrates its commitment to excellence through external accreditations against a wide range of industry standards, including the National Safety and Quality in Healthcare Services (NSQHS) Standards, Aged Care Quality and Safety Standards, Diagnostic Imaging Standards and Pathology Standards.
The NSQHS Standards are the over-arching standards. Eastern Health underwent an organisation–wide NSQHSS assessment and was fully re-accredited by the Australian Council on Healthcare Standards (ACHS) against these NSQHS Standards in 2023. The next Eastern Health assessment of these standards is changing Australia-wide to short notice (24 hour) assessments from the 1st July 2023.
A range of Eastern Health’s services are accredited by the Australian Aged Care Quality and Safety Commission, including our two residential aged care homes – Monda Lodge and murrenda Residential Aged Care Home and the Transition Care Program. murrenda was re-accredited by the Commission in July 2023 for another three years within 9 months of its opening and transferring of three existing Eastern Health homes into one purpose built state of the art home.
In 2022/23, Eastern Health continued its commitment to providing high quality care closer to home. Supported by the state government’s Better at Home program, Eastern Health saw sustained growth in bed substitution services (for example, a 23% increase in subacute separations via @home services), reductions in avoidable hospital presentations (for example, a reduction in readmission rate for community rehabilitation consumers from 13% to 3%) and improved access (for example, a 19% growth in Oncology at Home activity, driven primarily through telehealth models of care). The Better at Home initiatives introduced/sustained through 22/23 supported consumers to remain well at home, thereby reducing the demand upon hospital-based resources. The Better at Home program will continue into 23/24, with a renewed focus on digital supports to enable models of care and partnerships with community health services to support chronic disease management.
As a result of the COVID- 19 pandemic, there was a significant reduction in the number of elective surgeries performed across Victoria. During the pandemic this ranged between 25-75% of usual activity. Subsequently, there has been a profound effect on elective surgery waitlists.
As a response to COVID-19, Health Service Partnerships (HSPs) were formalised in an effort to foster collaboration in the Victorian health system, share best practice and harness scale across regions. Elective Surgery is a priority reform area for the Department of Health and is being progressed through HSPs.
Eastern Health is part of the North East Metro Health Service Partnership (NEMHSP).
Eastern Health is part of the North East Metro Health Services Partnership which has been collaborating to transform elective surgery with the aim of improving patient experience, optimising access and efficiency of care whilst keeping patients safe.
|
You said (the patient) |
We did (what actions we have taken from the feedback) |
| The wait time for elective surgery is too long. |
Developed or expanded a number of clinics to target non-surgical care, provide a better patient experience and divert patients from surgical waitlist. Established a multidisciplinary preoperative high risk surgical clinic to:
Enable seamless transition of care to the hospital team, including appropriate handover of clinical information Converted several procedures to ‘day cases’ thereby improving access and patient experience. Implemented ‘Enhanced recovery after surgery’ (ERAS) models of care. ERAS is a multidisciplinary, patient-centred and evidenced based framework that aims to optimise the perioperative journey, reduce surgical stress response and facilitate recovery to enable earlier discharge home. Implemented Fast Track Reassessment of long-wait patients. Patients who have been waiting the longest time on the elective surgical waitlist have been contacted and re assessed to establish the best plan for them. This has also assisted in progressing the patient journey to surgery or diverting to other conservative pathways. |
