The 2021-2022 Quality and Safety Highlights provides a snapshot to the community on Eastern Health’s quality and safety outcomes.
A full summary of the 2021-2022 financial year can be accessed via our 2021-2022 Annual Report.
Patient Experience
Eastern Health hears the voice of the patient, families and carers in a number of different ways. Patients, families or carers can:
- Speak with any staff member or the manager from the area where the experience occurred;
- Call, email or write to the Centre for Patient Experience;
- Use feedback forms in feedback brochures found in patient areas;
- Use the online feedback form on the Eastern Health website;
- Publish your experience without giving your name on the online public platform Care Opinion; and
- Complete the Eastern Health Patient Experience Survey available on discharge.
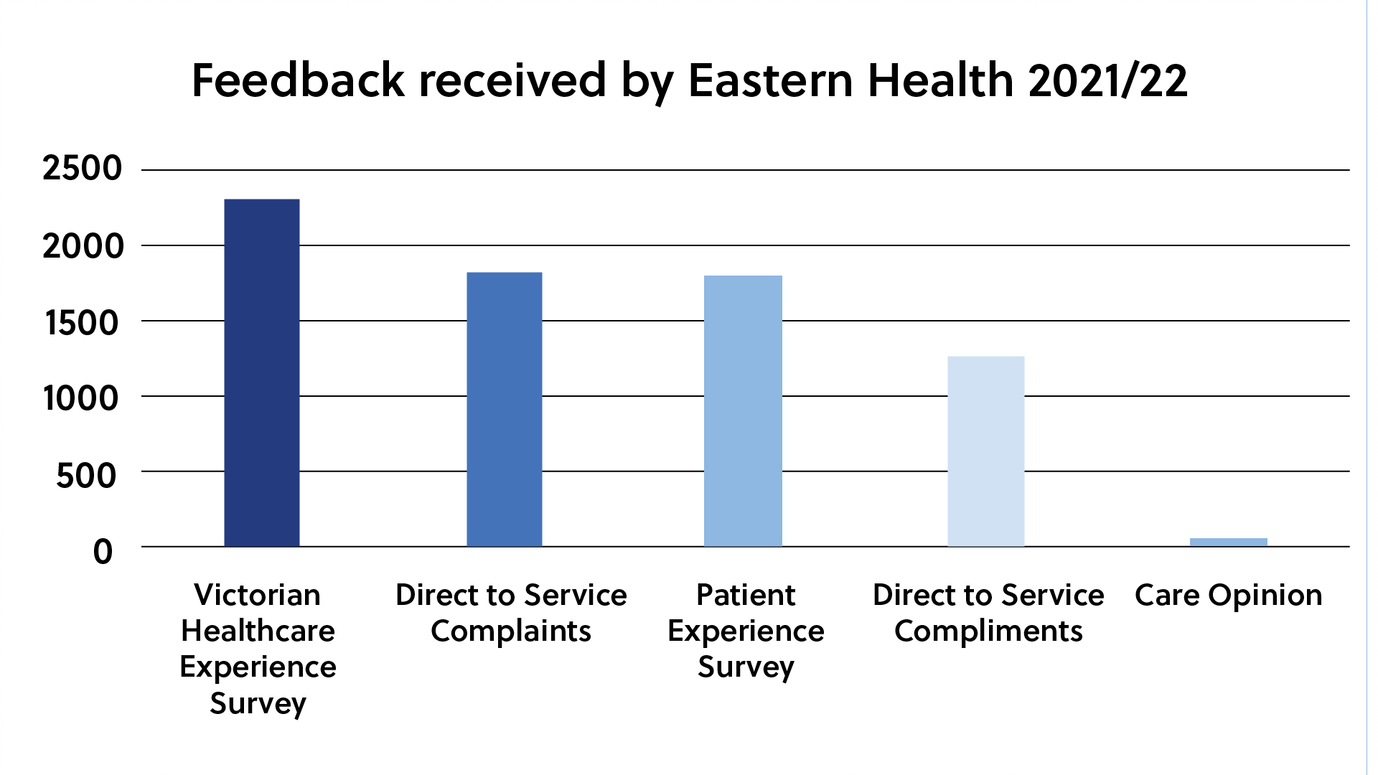
There were 7,267 items of feedback received by Eastern Health in 2021/2022. The mechanisms used for feedback in the past year are shown below.
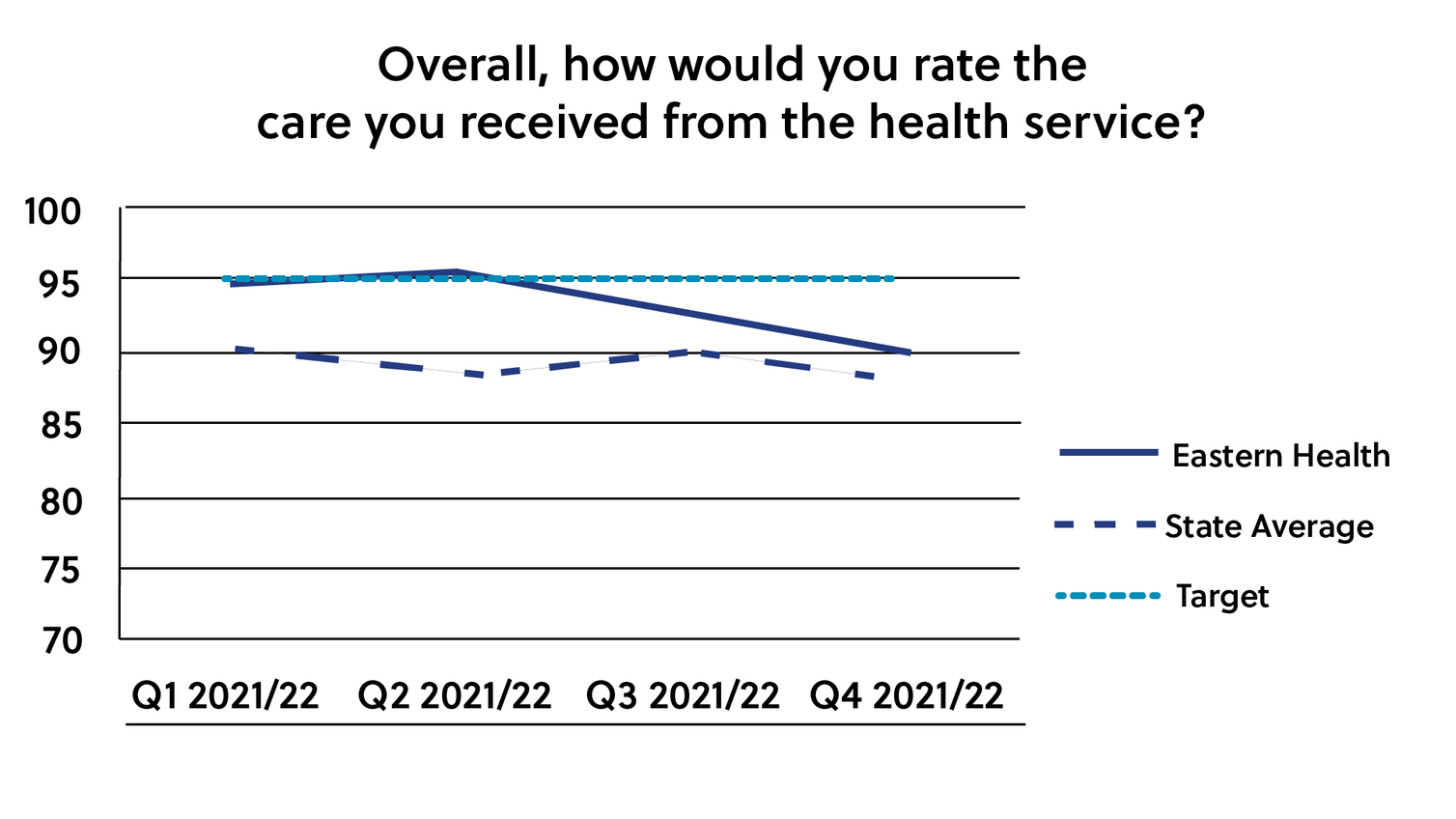
The Victorian Healthcare Experience Survey (VHES) is one of the ways patients can provide feedback about their experience with Eastern Health. The VHES collects information from a range of healthcare users of Victorian public health services. The survey is conducted by Ipsos (on behalf of the Department of Health and Human Services), and invites feedback from patients after discharge from the health service. The table below provides responses from adult inpatients at Eastern Health during 2021/22 to the question “Overall, how would you rate the care you received?”. Eastern Health performed above the state average for the three quarters provided. April – July data for 2022 is yet to be received.
Eastern Health uses feedback from patients to identify opportunities to improve our services and the experience of patients, carers and families. Below are some examples of taking action based on feedback provided by consumers.
| You said (the patient) | We did (What actions we have taken from the feedback) |
|---|---|
| Clients have concerns over the welfare of their beloved pets, with no one often able to look after them when they are admitted to Wellington House to improve their health and get clean and sober. |
Our newest peer worker Jess contacted all the charitable animal organisations in and around Melbourne, asking if they had capability to look after clients’ animals, or find a “respite” home until they are discharged from Wellington House. This resulted in Jess developing a list so that staff could contact such organisations, relieving pressure and unnecessary stress for the clients about the welfare of their precious fur babies during their inpatient stay. This was a really great initiative and one in which both clients and staff were so happy to be involved. Turning Point |
| Your staff are not well skilled in the use of the MegaBee device (an assisted writing tablet to aid frequent communication with people who have no or impaired, ability to speak and cannot write legibly) to help patients like me paralysed from Guillain-Barré Syndrome communicate. |
We underwent a review of our strategies to help patients like this. We concluded that all members of our team should indeed be more comfortable and adept at using the MegaBee. We produced a carefully edited instruction video and incorporated this in an iLearn course that has subsequently been completed by 96% of our front line ICU staff. We are much more likely to reach for the MegaBee now and many patients have benefited. Perhaps the best example of this is John and his family. John was recently in Box Hill ICU where he suffered through 2 months of agonising whole body paralysis. For much of this time, he was fully awake and aware. The team quickly reached for the MegaBee, which rapidly become John’s primary way to interact with everyone – nurses, doctors, PSAs and even his family. In fact, we gave John’s pregnant wife our instruction video and she rapidly became the most capable MegaBee user we have ever worked with. John and his family are incredibly grateful for the work our team has put in to get as comfortable as we have with the Megabee. Much of the credit for this happy story is owed to the patient who first gave us the critical feedback. Intensive Care Unit, Box Hill Hospital |
| The queue for COVID-19 testing is too long and there is nowhere to sit and limited opportunities to get out of the sun. |
We implemented a ticketing system which provided an allotted time slot for those requiring testing to come back and be tested. This meant people could choose to go home and return in their allocated time, reducing the time spent in the queue. Multiple sites |
Partnering with Consumers
Information underpins everything we do. The “Partners in Care – help us to care for you during your hospital stay” booklet provides important information on how we can partner together to care for you during your hospital stay. The booklet includes information on involving you in decisions about your care as well as the things you can do to decrease the likelihood of known risks including falls, pressure injuries and infections.
| You said (the patient) | We did (What actions we have taken from the feedback) |
|---|---|
| We want key information available in a printed brochure and we also want it available in other formats we can access on a personal device. |
In 2022, the Partners in Care video was launched to provide this information in a different way. The video is available on the Eastern Health website and via a QR code in the Partners in Care booklet and a QR code on Partners in Care posters displayed in patient areas. |
Shared decision making
Working in partnership and ensuring you have the right information and support to make decisions about your healthcare is very important to us. This short video provides a consumer perspective on what “shared decision-making” means to them. This video is used in providing training to staff.
| You said (the patient) | We did (What actions we have taken from the feedback) |
|---|---|
| Sometimes I leave my health appointments feeling I haven’t really understood things. I feel unsure about what I need to do next and find it hard to remember exactly what I was told. |
Eastern Health has promoted Check-back, an externally developed resource which involves patients checking-back with the clinician by repeating what they just heard in their own words. That is, by saying to the clinician something like: “Let me just check I understand, did you say…..”. Eastern Health held a focus group attended by 10 consumer representatives to inform consumers about the Check-back campaign, try and understand if the campaign would meet the needs of the consumers and explore ways to implement the campaign. The consumer representatives were very supportive about implementing Check-back and provided great ideas regarding implementation which has led to the creation of a poster and communication via Eastern Health website and social media sites. Information on Check-back can be found at www.checkback.org |

Eastern Health’s Rainbow eQuality demonstrates Eastern Health’s commitment to ensuring a safe workplace and to being an inclusive provider of healthcare for all lesbian, gay, bisexual, transgender, gender diverse, intersex, queer and questioning (LGBTIQ+) people. This working group has supported a number of initiatives including:
- Sponsorship of and participation at the Pride Cup in 2022;
- Coordinating communication and acknowledgment of IDAHOBIT Day (International Day Against Homophobia, Biphobia, Intersexism and Transphobia);
- Ongoing work to address the recording of sex, gender and sexuality on patient information systems;
- Ad hoc training and awareness sessions to address issues raised by patients and staff regarding the needs of LGBTIQ+ people.
| You said (the patient) | We did (What actions we have taken from the feedback) |
|---|---|
| I don’t identify as Mr, Mrs, Ms or Miss and do not want to be recorded as one of these options in your information systems. | The title “Mx” is now available to be used to record a patient’s title in our patient identification systems. We continue to advocate for further changes to state-wide patient identification systems to enable systems to be more inclusive. |
In 2021/22, the Eastern Health Disability Working Group has continued to undertake work to oversee and support the implementation of actions on the Disability Action Plan. Eastern Health’s disability liaison officers have supported the working group with key achievements in 2021/22 including:
- Working with 1,542 people with a disability in the east to help them access health and COVID-19 services;
- Helping people with a disability access COVID-19 (and flu) vaccinations by establishing supported vaccination clinics and sessions at mass vaccination hubs, low sensory clinics, specialist development schools and in the home, and by providing sedation support to administer vaccinations;
- Reducing barriers for inpatients to access NDIS support enabling them to leave hospital sooner with better outcomes;
- Providing RATs and N95 masks to people with a disability in the community and assisting them to access in-home PCR tests and early COVID-19 treatment;
- Providing education to over 250 Eastern Health staff to raise awareness of the needs of people with a disability in health, especially in the area of neurodiverse care; and
- Presenting at local, state and commonwealth forums to promote the disability liaison service, raising awareness of needs of people with a disability when accessing health and COVID-19 services and advocating for support.
| You said (the patient) | We did (What actions we have taken from the feedback) |
|---|---|
|
My child has sensory needs and cannot be vaccinated at a mass vaccination hub or busy GP clinic.
|
Established a low sensory clinic in the region and in-home and in-school vaccination options with partnering organisations. |
| I want my access needs to be known if I need to come to hospital (NDIS participant with complex needs). | Emergency departments were made aware and care plans were uploaded on the patient file. Information was used at the first presentation and very helpful for person and staff. |
Family violence training modules have been made available to Eastern Health staff via our online learning portal so that staff are trained to identify and respond to patients, their families and even colleagues who are experiencing family violence. This helps Eastern Health align to the state-wide MARAM (Multi-Agency Risk Assessment and Management) framework and information sharing schemes legislation. Eastern Health’s commitment to family violence response has extended to making the training mandatory for all staff.
Eastern Health has also worked towards building collaborative relationships with staff at the inner and outer East, Orange Door which are the newly implemented ‘one door’ service that responds to family violence and child wellbeing in our region. Together, Eastern Health and the Orange Door staff can provide a collaborative response to family violence victim survivors, as well as people who use violence.
ELSA (Engaging & Living Safely & Autonomously) – a health justice partnership between Eastern Health and Eastern Community Legal Centre
For our older patients, we have partnered with ELSA to provide additional support for any legal concerns. Engagement in ELSA services is voluntary – nothing happens without the patient’s consent. The ELSA community lawyer and financial counsellor can discreetly meet with the patient while they are in hospital or receiving care from Eastern Health services to provide free and confidential advice, support and information about their legal rights and managing any financial difficulties. Patients can access these services by asking Eastern Health staff members to make a confidential referral to the ELSA team.
Consumer representative participation
We encourage patients, carers, family members or community members to join our consumer register as a consumer representative – we currently have 91 consumer representatives coming from all walks of life partnering with us. Consumer representatives are provided with opportunities to bring the patient voice to improve our healthcare services at Eastern Health through committees, working and focus groups, research, improvement projects and staff training including:
- Opioid Analgesic Stewardship Committee
- Mental State Deterioration Working Group
- Use of a digital app to enhance patient-centred nursing handover
- Co-design – evaluating the efficacy of a digital app
- Cleaning audit
- Clinical governance quality systems training; and
- Strategic plan development.
Integrated Research: an example of where consumer representatives were involved in research
When patients are in hospital, doctors and nursing staff change shifts at least once every 24-hour period. When those shift changes occur, those going off shift need to hand over information about the patient’s condition to incoming staff clearly and accurately, or something could go seriously wrong.
Eastern Health has worked with some of our consumer representatives on a research project to find a way of improving communication between nursing staff and patients during handover. The research team, nurses, consumer representatives and Deakin University put their heads together to develop a digital app for patients and nurses to use during handover at the bedside:
- Patients will receive an iPad where a digital app will be installed with their basic information (name, date of birth, etc.);
- Patients will be able to see names of the nurses looking after them on the iPad; and
- The iPad will always remain with the patients and they will be able to write questions that they would ask the nurse at handover. For example: When will I receive my blood tests results?
Consumer representatives and volunteers were involved as ‘patient actors’ together with nurses in simulation workshops to test the digital app during a handover at the bedside.
Eastern Health’s response to the Royal Commission into Victoria’s mental health system
In February 2019, the Victorian mental health system was described by many as ‘broken’ and failing to support those who needed it most. In 2020/2021, a Royal Commission was established to engage people with a lived and living experience of mental illness, their families, carers and supporters, mental health workers, researchers, service providers and others. Eastern Health welcomed the opportunity to be part of the process.
The Commission’s recommendations were centred on transformational reform, with a vision for a balanced system where mental health and wellbeing treatment, care and support are provided in the community, hospital and other residential settings.
Development of Eastern Health’s Mental Health and Wellbeing Transformation Plan
Consultation sessions led by the Eastern Health Royal Commission project team were undertaken with a range of clinicians and lived experience workers from across our mental health program. Lots of valuable information was gathered through these discussions about how Eastern Health can best transform and address the Royal Commission’s recommendations and the eight initial priorities. The transformation plan was completed and submitted to the Department of Health at the end of June 2022.
- Read more about our response to the Royal Commission into Victoria’s mental health system
- Read more about our transformation plan and the eight priority areas being addressed
- We welcome any questions about Eastern Health’s Royal Commission response which you can send to the project team at: [email protected]
Quality and Safety Outcomes
An incident is an event or circumstance which could have resulted, or did result, in unintended or unnecessary harm to a person receiving care. While safety of patients, staff and visitors are taken very seriously and health services take all steps to ensure safety and quality of the services, sometimes things do go wrong. All Eastern Health staff are required to report incidents and potential safety issues so that we can learn from these events and reduce the likelihood of things going wrong. Eastern Health encourages and supports patients and families to provide feedback and these events are reviewed to identify opportunities to improve safety, quality and patient experience.
Each incident is rated according to degree of harm and changes to the level of care and treatment required as a direct result of the incident. This severity rating informs follow up of both the individual incident and system issues identified. Each incident is assigned a rating between 1 and 4, 1 being the most serious outcome to 4 where no harm has occurred but was a near miss.
All reported incidents are initially reviewed by the manager of the location where the incident occurred. There is an immediate assessment of safety and care of those involved and any identified concerns are addressed. Information is gathered from staff, patients and visitors at the time of the event to get a thorough picture of what has occurred.
All incident reviews apply the following key principles:
- Determine the timeline of events leading up to an including the incident.
- Identify if there are any issues or variations from expected practice.
- Identify what may have contributed to the issues.
- Consultation and communication with the patient/family to ensure a collaborative and informed process.
The most serious incidents are reviewed by a panel of clinicians, service providers and consumers.
Sentinel events are unexpected events that result in death or serious harm to a patient while in the care of a health service. Eastern Health notified SCV of 17 sentinel events during 2021/2022.
Graphic demonstrating incident numbers with and without harm.

Incident numbers by month
- Average of 1400 patient incidents are reported per month.
- Average 340 patient incidents resulting in harm are reported per month.
The three main incident types where harm has been experienced by a patient are:
- Falls – 3463
- Behaviours of concern* – 7422
- Skin integrity (for example, bed sores or skin breaks) – 794
*Behaviours of Concern are behaviours that people engage in which are unsafe and/or distressing to the person and/or others. This may include someone harming themselves, other people or things. These behaviours can be very stressful and upsetting. These behaviours can seriously hurt people.
The primary purpose of incident review is to understand how and why the incident occurred and to identify ways of preventing recurrence. Here is an example:
| What happened? | What did we do? |
|---|---|
| An elderly man presented to an emergency department from a nursing home with shortness of breath and decreased oxygen levels. Due to a likely COVID-19 infection, he was moved to an isolation cubicle (a specialised room where someone with a contagious respiratory infection can be managed). An hour and a half after presentation, the patient had a witnessed fall from standing height with head strike whilst a staff member outside the isolation cubicle was donning personal protective items such as gown, gloves, mask and goggles). The patient suffered a catastrophic bleed on the brain and died. |
Greater visibility of people in respiratory isolation is required. The emergency department will install a video surveillance system to augment patient visibility in low visibility/high acuity cubicles. |
In 2021/2022, Eastern Health saw significant growth in our capacity to deliver high quality, safe care in our consumers’ homes. Supported by the state government’s Better at Home program, Eastern Health implemented new home-based services across rehabilitation, neonates, cardiology, general medicine and chronic disease management and expanded existing ‘at home’ services such as the Early Supported Discharge for Stroke program and our Oncology at Home service.
With the establishment and growth of these services, more members of our community were supported to stay well at home, thereby avoiding clinically unnecessary visits to hospital. If a hospital admission is required, these new services also support timelier follow ups following discharge.
Eastern Health will continue its commitment to high quality, safe care outside the hospital walls, with further innovations planned for 2022/2023 and beyond.